Last week I reviewed the mechanics of two complex tendons, focusing on the function across many joints and in many areas. If you count them out, you can easily find 7 common areas of pain involved in a peroneus longus injury for example. As a presenting complaint, the patient may have pain in multiple areas all related to the same tendon. This is not counting the compensatory pains caused by the tendon not working properly, with muscle substitutions, pain from the injury inflammatory condition and pain from disuse atrophy if the problem has been chronic. I like to work on the inflammation, typically some nerve hypersensitivities, as much core and lower extremity strength through PT and Cross Training (if they can not walk, can they bike or swim for example). Slowly the pain does tend to generally localize to one area.
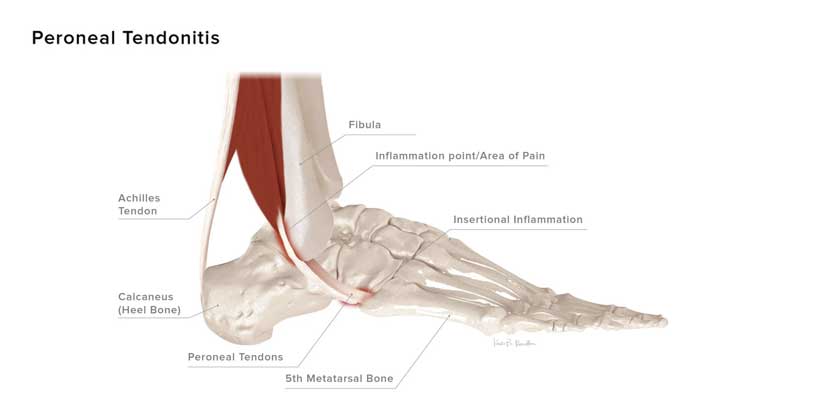
The general rule of thumb of peroneal problems is that it is often related to supination tendencies, and therefore treatment is for over supination. But, as I described last week, there are many functions of the peroneals that could be related to pronation tendencies. Even the simplest tendon, peroneus brevis, has a major function stabilizing the lateral aspect of the cuboid as the forefoot abducts from the rearfoot, and stabilizing the lateral side of the sinus tarsi another area impacted by pronation.
Tendonitis symptoms as a presenting complaint, and your working diagnosis, can just be compensation for a deeper bone or joint problem. Therefore, either peroneal tendon can present with roaring tendonitis symptoms only to discover that the fibula has a stress fracture, or the ankle has a OCD, or the cuboid has some degenerative arthritis involving one of its connecting bones. This concept may be important if your treatment for the tendonitis does not seem to be completely helping, always think deeper.
So we have 2 tendons that can be overworked and strained by either pronatory stresses or supinatory stresses. These functions usually require different orthotic devices for sure. I LOVE TO WATCH THE PATIENTS WALK. Do I see them pronating too far, or have a tendency to supinate or live more on the outside of their foot with no pronation seen? I LOVE TO TAKE MEASUREMENTS. Which may not be your cup of tea? They help me decide the patient's heel position at least. A patient who stands with the heel vertical or 2 inverted is more prone to supinate in gait than a patient who is 14 degrees everted. You can also ask the patient if they feel like they move through their feet heel to the big toe, or roll outward too much or pronate too much.
So, let’s take a patient with peroneal tendonitis with no abnormal tendencies. Here is the KRM recommendation based on diagnosis with 2 additional modifications for the lateral column.
So, let’s take a patient with peroneal tendonitis with definite supination tendencies. I would start with this: Root Control for lateral ankle instability and add a lateral frame fill (Denton modification)
So, let’s take a patient with peroneal tendonitis with definite pronatory tendencies. The starting point would be: P12 - Pes Planus, but I would remove the forefoot post and add a medium lateral flange and lateral frame filler.
Next week I will dive deeper into this fun topic.





