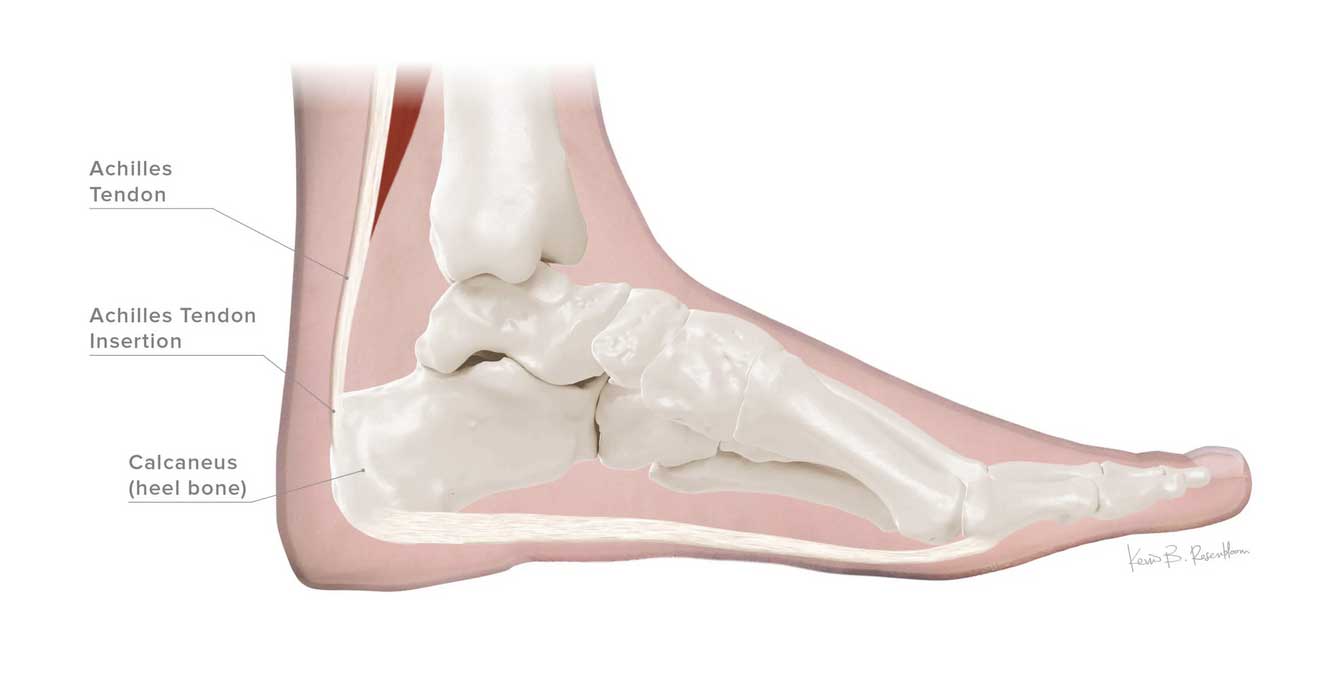
The Achilles Tendon is definitely something that you could specialize in your practice. Being the strongest tendon in the universe, its effect on the body is immense for allowing us to evolve to an upright position, for stability and for movement. You can approach the achilles tendon passively or proactively. By passively, I mean only thinking about it when a patient presents with pain in the achilles and you are forced to do something. By proactively, I mean to say that evaluation of the biomechanics of this important tendon, and treatment of any abnormalities found, even when the patient presents with another issue, can really improve a patient’s active lives. I know I am bordering on preventative medicine, and this may not be your thing, but here goes.
What are the standard biomechanics of the achilles tendon that we can influence? These include:
- Overall strength of both the gastrocnemius muscle and the soleus muscle
- Overall flexibility of both the gastrocnemius muscle and the soleus muscle
- The heel drop of their current workout shoe(s) and for various activities
- The subtalar joint neutrality or degrees from neutral (frontal plane) that they are functioning in when doing repetitive motion activities
- The degrees and duration from ankle neutrality as they participate in non-walking activities
- The amount of limitation of the first MPJ at heel lift
- The asymmetry of function due to particular activities, asymmetrical foot design/deformities, short leg syndrome and compensations
- And, other factors affecting the speed of movement, the ballistic nature of an activity, the duration of an activity especially when the achilles is not in a good position, etc.
So how do we begin to make both sense of this and treat our patients better? I hope you remember the Rule of 3. Since every foot can have different needs, finding 3 things that can help any situation typically means that you will find an important cause of an injury, and treatment modality for that injury. For some patients, it is their flexibility from too tight or hyperflexibility that they will need to work on. For others, it is their strength, especially in overall basic tone, and then the demands of an activity and fatigue that may set in. For others, it will be the heel height of their shoes we can control, as zero drop shoes and negative heel positions place extra strain on the achilles tendon in repetitive motions. Subtalar neutrality means the ideal positioning of the ankle tendons and variations from this position in repetitive motion activities can cause either pronatory or supinatory moments that can strain the tendon(s). An inability to have a smooth and symmetrical heel lift and subsequent push off due to lack of appropriate big toe bend can easily irritate the achilles as it attempts this important function. The body is also always trying to move symmetrical, so deformities or functional problems that produce asymmetrical function can really produce strain. This does not have to be completely eliminated, but working in the direction of symmetry with lifts for short limbs, asymmetrical orthotic Rxs, or changes in activity patterns (like running a banked track every other day in the opposite direction) can be hugely beneficial. Next week I will begin to break these down for you. But, in summary, improvements in the following 6 categories can greatly help function and reduce future injuries (and allow you to achieve “genius” status with your patients):
- Flexibility improvements
- Strength improvements
- Biomechanical improvements, especially in asymmetry
- Shoe improvements with higher heel positioning
- Activity changes with less deviations from ankle neutrality in repetitive motions (like less consistency in running up and down hills day after day)
- Improving any functional hallux limitus found





