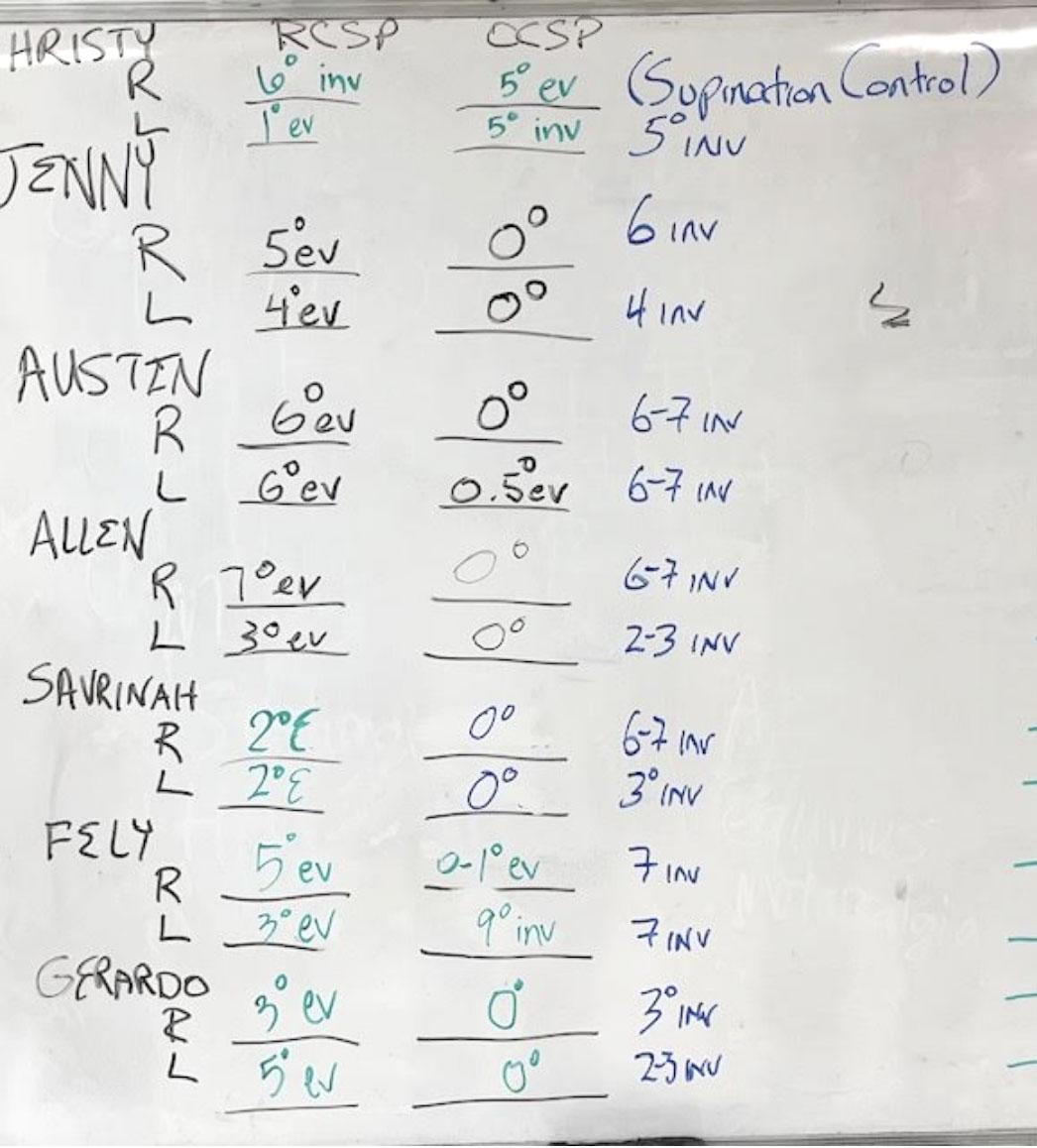
Recently my students at Samuel Merritt’s College of Podiatric Medicine received their orthotic devices to begin to break in. I want to go over the orthotic dispense ritual and our findings and Rxs over the next 3 posts. To me, the 7 students in the class were the typical patients you see in the office with 6 pronators (mild, moderate, and severe) and 2 supinators (and only on one foot—right side). Here is the graph of some of the measurements I need for this visit—RCSP and OCSP, with MPP and NCSP measured in the last class, followed by gait evaluation. Only one of the seven students had enough signs of limb length (around ½ inch), that I also started on lift therapy once orthotic break in was completed. Next post, I will add to this NCSP and MPP which I think really round out a good biomechanical assessment for Rx writing.
The first thing that the students must do for the 2 important measurements above, and MPP and NCSP, is to bisect the heels of their fellow classmates. Even though this is an easy task for them, I always check for accuracy and all 14 heel bisections were right on (with an occasional crooked line). I was very proud of them. Dr. Timothy Dutra teaches them this skill and does an amazing job.

The posterior surface of the heel is bisected and our measurement will be undertaken. Here the student stands in RCSP with everted heels (heel valgus position).
Then we stand the students up in angle and base of gait, and measure RCSP. RCSP is the first column of numbers after the students' names. All the students first stand back and look at their classmate’s posterior heel. With the heel bisected, I make them tell me if the line drawn represents heel verticality or 0 degrees, an everted heel or an inverted heel. And, I make sure these 2nd year students are seeing it correctly. Then, they put degrees onto those observations with the use of goniometers, prolevels, and phone apps (to check consistency). You can see that everyone had everted heels (13/14) except Christy’s right foot that was inverted.
The second, or middle column, is made right after the RCSP and is called OCSP or Orthotic Calcaneal Stance Position. I thank Dr. Kevin Kirby for really emphasizing the importance of this measurement to document static improvements. You are always having to make sure what you are seeing statically is actually occurring dynamically in your gait evaluation and your feedback from the patient. All patients responded in the direction the prescribed orthotic was supposed to, however 2 of the 14 feet made me think more (to be discussed later). Can you pick out these 2 feet that I will discuss in the next few posts? (Hint: Christy’s right and Fely’s left)
I will finish today explaining the 3rd column in blue. The 3rd column represents the change I asked the orthotic device on each foot to make by my prescription. The prescription writing for exact degree changes is an average, so patients can respond more or less degrees from this average, and you have to decide if you want to make changes to the original orthosis or order a new and improved version down the line. Therefore, only one patient we ordered a device to control supination and for only one foot, with the other 13 feet having various degrees of inversion correction ordered for their everted heels. If you refer back to my discussions of all the corrective foot orthotic devices out there, I used one of the S (supination control) orthoses, and 13 of the P (pronation control) orthoses. We will discuss next week the orthosis I used on Christy’s right foot, but it was a cross between S1 and S2. The P orthoses are all over the place with a 7 degree correction being the highest I will start a patient. With each degree giving 1/16th inch support, a 7 degree correction is 7/16 or very close to 1/2 inch.This big change at the foot takes time for the body to adapt to. This adaptation is better in younger patients, so my very young students should be good to go.
Next week I will add in the MPP and NCSP for each which we measured in the session before. My objective is to get my readers at orthotic dispense to do the following:
- Perform a heel bisection
- Measure RCSP
- Measure MPP
- Measure NCSP
- And then measure OCSP
This will give you a great idea of how a patient is statically positioned in your orthotic devices. Of course, you then perform OGA (observational gait analysis) or CAGA (computerized assisted gait analysis) to verify your results. What is happening dynamically can be different than statically, but usually not for the walking gait cycle. This approach has helped me with tens of thousands of patients. As we discuss each patient, I will highlight the KevinRoot Medical orthosis that I used to achieve these results.





