First of all, Drs.Hillstrom are my friends so I want to shout out to them. This article is a a fine example of their excellent work which I will summarize here. The instruments alone are worth the look. If you are unaware of the excellent works of Dr. Howard Hillstrom and his team, you are in for a treat. Here are some of the points that they bring up. They are:
- They chose a definition of hypermobility as greater than or equal to 8, whereas Dr Root 60 years ago settled on greater than or equal to 7. This of course is the dorsal excursion of the first metatarsal in the sagittal plane only in relationship to a fixed 2nd metatarsal head. So, we basically have a 1 mm change in these 60 years.
- They concluded that 86% of patients with pes planus also have first ray hypermobility. This is quite a correlation and never adequately documented until now.
- Here are the static foot structures that they looked at: 1) arch height flexibility, 2) weight bearing first ray mobility, 3) first metatarsal phalangeal joint mobility, and 4) first ray mobility (with greater than or equal to 8 mm of dorsal excursion indicating hypermobility).
- Whereas, planus feet correlated to first ray hypermobility, the other measurements did not. However, they did find a link among these other 3 measurements. They were trying to tie first ray mobility to first MPJ flexibility.
- Therefore there was some link between weight bearing first ray mobility (machine measured) and the two that we could measure first metatarsal phalangeal joint laxity and partial weight bearing first ray mobility (our functional hallux limitus test).
- The examiners used a device called the “Arch Height Index Device” to categorize the patient’s foot type. The article tied to this by Dr. Howard Hillstrom and Dr. Jinsup Song, et al is fascinating and another article to review.
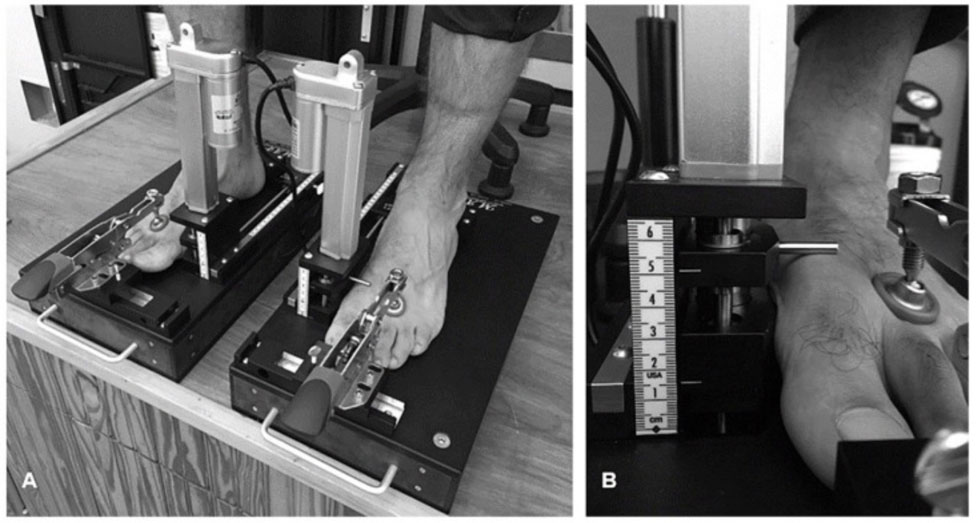
- Another device called MAP1st was used to determine first ray hypermobility.
- Their study clearly linked pes planus to first ray hypermobility at an 86% rate, therefore, if you had a hypermobile first ray you most likely had a pes planus foot type.
- However, their study also found that 42% of pes planus did not have first ray hypermobility, it is just a general rule that must be individualized in your treatment of patients. Therefore, of all the pes planus patients, only 58% have a hypermobile first ray.
- The two standards in the industry for the treatment of first ray hypermobility and its weight bearing shifts away from normal and over pronation tendencies are Morton’s extensions and functional foot orthotic devices to control the pronation of the foot.
- The goal of the Morton’s extension is to allow the first metatarsal to bear weight by bringing the ground up to it, and not to jam the first metatarsal further dorsally. The patient should feel more stable, observed gait should be more stable, and symptoms associated with the hypermobile first ray should be improved. This may not work if the patient is not well controlled in the medial arch and continues to have over pronation issues. And, this may not be needed in cases of hypermobile first rays only related to over pronation and not part of the patient’s foot structure.





